
Phil
Cleverley
SCOR Chief Underwriter
September 27, 2023
It is now over 40 years ago that Acquired Immunodeficiency Syndrome (AIDS) was first described, and the Human Immunodeficiency Virus (HIV) was identified as the cause. Since that time, it is estimated that globally over 85 million people have been infected, over 40 million people have died, and it is currently estimated that there are 38 million people living with HIV globally. However, there have been tremendous advances in understanding the condition and developing treatments that have dramatically changed the outcome for those infected and that will reduce the number of infections in the future.
From an insurance perspective, HIV has always presented a challenge from the early days when there was much uncertainty relating to how significantly it could impact upon mortality and morbidity, and subsequently to ensure underwriting guidelines were aligned with continuous and often fast-moving medical developments.
At SCOR, we have always endeavoured to ensure that our underwriting guidelines for HIV contained within our SOLEM manual were reflective of current evolutions and we are shortly to release updated guidance, with much improved acceptance terms across all major types of protection products including life cover, critical/serious illness, and disability related products.
We are also taking the opportunity to significantly improve the accompanying information pages included in SOLEM, to help underwriters identify the important risk factors associated with HIV.
This article includes information that has influenced the changes we are making to SOLEM and provides background to help the evaluation of HIV risks for underwriting and claims assessment.
HIV is a retrovirus of two types (HIV-1 and HIV-2) that attack the body's CD4 T lymphocytes (the cells that guard against assault by viruses, fungi and other organisms) and weakens the immune system. HIV-1 is the most common and virulent type, responsible for the majority of HIV infections worldwide.
AIDS represents the most advanced stage of HIV infection, characterised by severe immunosuppression and an increased risk of opportunistic infections and certain cancers. The criteria for AIDS classification include the
The most significant factor that has had the most impact upon mortality and morbidity improvements was the arrival of effective treatment in the form of Highly Effective Antiretroviral Treatments (HEART or ART) that became available during the 1990’s.
ART transformed HIV from a universally fatal infection into a long-term manageable condition with the inevitable rise in global prevalence. ART has also played a huge role in reducing transmission of HIV by suppressing the activity of the virus in individuals to a level making it far less likely they can pass it on to others.
PrEP is a preventive approach used to reduce the risk of acquiring HIV infection in individuals who are identified as being at a higher risk of getting HIV. PrEP involves taking antiretroviral medications on a regular basis and has been found to be highly effective.
PrEP is now freely available in the UK and Ireland following the World Health Organisation’s recommendation in 2015 as a measure to further reduce transmission rates of HIV.
It is recommended to use PrEP in combination with other prevention strategies, such as consistent and correct condom use, regular testing for sexually transmitted infections, and behavioural interventions to reduce risk.
As a result of PrEP and ART, transmission rates in the UK and Ireland for HIV are very low and are likely to improve even further in the coming years.
In 2014 the United Nations Programme on HIV/AIDS (UNAIDS) established global targets to scale-up HIV treatments with the intention of ending the HIV epidemic by 2030. These “90-90-90” ambitions are as follows:
Despite great strides in the availability of prevention tools and effective treatment, the response to the global human immunodeficiency virus (HIV) health crisis remains suboptimal and continues to impact some of the world's most vulnerable populations. The coronavirus(COVID-19) pandemic also increased health inequalities even further. Therefore, some regions still have a long way to go to meet the UNAIDS targets.
In 2019, it was estimated that there were 105,200 people living with HIV in the UK.
Of all the people living with HIV in the UK, 89% are virally suppressed. However, there is some lack of clarity over the number of people lost to care.
There are over 7,000 people who are estimated to be living with HIV in Ireland. It is estimated that about 10% of those living with HIV in Ireland don't yet know they have HIV, because they have either never had an HIV test, or they got HIV since their last test. Since 2015, around 500 people are testing positive for HIV in Ireland every year. Of these, around 40% are people who had a previous HIV diagnosis abroad.
Viral load and CD4 count are two crucial measurements used in HIV management to assess disease progression, monitor treatment effectiveness, and guide clinical decisions. Viral load refers to the amount of HIV RNA (genetic material) present in a person's blood plasma. It is measured using a laboratory test called a quantitative HIV RNA assay.
With successful treatment, viral load can be attained to a very low level, which keeps the immune system working and prevents illness. This is called viral suppression and is defined when levels are controlled at a certain level (usually 200 copies of HIV per ml of blood). It is also possible to achieve a viral load so low that a test can’t detect it. This is called an undetectable viral load and is below 20-50 copies/ml.
CD4 count refers to the number of CD4 T lymphocyte cells in a person's blood. CD4 cells play a critical role in maintaining the immune system's function.
Viral load and CD4 count are interrelated, and monitoring both provides a comprehensive view of HIV disease progression and treatment response. The goal of HIV management is to achieve sustained virologic suppression and maintain CD4 counts at levels that reduce the risk of opportunistic infections and other complications.
Regular monitoring of viral load and CD4 count is important to guide treatment decisions and optimise HIV care. These measures are equally important as underwriting considerations and are always required as part of the evidence requirements at underwriting.
In the UK, the monitoring procedures for those who have been diagnosed as having HIV is determined by the British HIV Association (BHIVA) guidelines, that detail ongoing tests requirements of those at all stages of HIV, from newly diagnosed to those with AIDS related conditions.
The latest BHIVA guidelines for those with HIV who are stabilised on ART with supressed viral load are as follows:
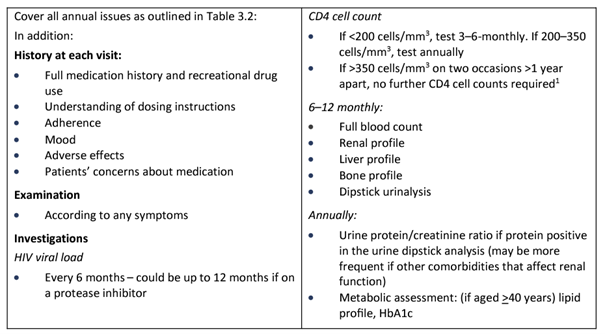
This provides useful information that can be requested at underwriting. What is important to note is that whilst viral load is measured on at least a yearly basis, it is now considered that yearly CD4s are no longer necessary when they are over 350 mm³, provided viral load is satisfactorily supressed.
In addition to ensuring adequate control of HIV, this monitoring is important to ensure there are no additional medical conditions arising and that the ART is being effective without any complications.
In Ireland, it is likely most people with HIV will be monitored according to European guidance provided by EACS. This is similar to BHIVA, although there are some differences and in particular the recording of CD4 on at least a yearly basis, even for those cases with stable and undetectable viral loads.
A viral “blip” is a reference to a short-term increase in viral load in someone who generally maintains an undetectable viral load, meaning that the amount of HIV in the blood was still low, but high enough to be detected by the viral load test usually to 60 copies/ml to 150 copies/ml and sometimes even higher. However, a viral blip is not necessarily an indication that treatment is failing.
Blips may occur due to variations in laboratory processes or having an infection like a cold or the flu. Some studies have suggested that these blips occur due to a release of the virus from reservoirs within the body and are not an indication of ongoing virus replication. However, if the viral load stays above detectable on two consecutive tests it would lead to closer monitoring and investigations with a view to possible change in treatment regime.
There are continuous studies being released that demonstrate the clear advancements being made in life expectancy for those with HIV. An important recent example was a study published recently in the Lancet(1) that claims to have produced one of the most detailed analyses of life expectancy among people living with HIV in high-income countries.
This research included 206,891 people with HIV from Europe and North America. One group of participants had started ART between 1996 and 2014 and were still alive and on treatment in 2015, when follow-up data began to be collected. Another group of participants started ART between 2015 and 2019 and subsequently survived for at least a year, when their follow-up data began to be collected. The 2015 cut-off was chosen as this was when treatment guidelines changed to recommend treatment for all people diagnosed with HIV, regardless of CD4 count.
The authors calculated life expectancies for the participants based on whether they started ART before or after 2015 and how they acquired HIV, as well as viral load, AIDS status, and CD4 count at the start of follow-up.
For people starting treatment before 2015, the average life expectancy for those currently aged 40 was 76 years for women and 75 for men, compared to 86 and 81 in the general population respectively.
The tables that follow show some examples from the study of life expectancy taking into consideration different risk factors:
Whilst studies show an increasing improvement in mortality, there is still an overall increased risk associated with HIV. The most serious complications of HIV infection relate to circumstances where AIDS develops from the risk of the many types of AIDS defining illness and opportunistic infections. However, there are also other complications associated with HIV.
HIV is known to cause chronic inflammation the levels of which generally decrease when ART is commenced. However, low levels of chronic inflammation tend to persist, that over time increases risks for health conditions such as cardiovascular disease, kidney disease, diabetes, bone disease, liver disease, cognitive disorders, and some types of cancer. This phenomenon was the subject of a paper written by SCOR in 2016(2). Studies have also shown that these conditions occur much sooner than those without HIV(3).
Other less common risks can relate to complications form ART and non-compliance. Indeed, the longer-term impacts from ART are only just now being revealed.
Whilst there have been significant improvements in mortality for people with HIV, studies continue to show they present a very significant risk for disability, particularly relating to the earlier onset of chronic disease (3).
This is particularly relevant when considering HIV risk for disability related products and critical/serious illness covers.
Whilst the incidence of HIV is reducing and treatments are improving, from an underwriting perspective, great care needs to be taken in view of the complexities involved. Therefore, it is vital that the appropriate medical evidence in the form of a general practitioner’s report or from the applicant’s HIV clinic is obtained that includes full details relating to the important risk factors.
The minimum detail required verified by medical evidence would be results of latest follow-up, including latest viral load and CD4 counts, control of condition and compliance with treatment. Also, any other co-morbidities and complications must be very carefully evaluated as acceptance terms will vary considerably upon these factors.
Plans are in place to end the HIV/AIDS epidemic across the globe and in developed countries including the UK and Ireland, there has been substantial progress towards meeting this goal.
HIV and AIDS has always been a challenge to underwriting, and less so for claims assessors where thankfully some of the predictions in the early days of the discovery of HIV of excessive claims did not materialise. It has also always been a high-profile condition that has needed to be handled carefully by the industry and underwriting acceptance terms have always been under close scrutiny by many stakeholders, including HIV support groups, regulatory bodies (including the Association of British Insurers and Insurance Ireland), brokers and those living with HIV.
The new SCOR guidelines for HIV provide improved acceptance terms across all protection benefits that reflect the latest medical advancements and are supported with a strong evidence base. Importantly, the new guidelines will enable more people with HIV to obtain the protection products they need.
(1) Trickey A et al. Life expectancy after 2015 of adults with HIV on long-term antiretroviral therapy in Europe and North America: a collaborative analysis of cohort studies. The Lancet HIV 10(5): e295-e307, May 2023.
(2) SCOR inFORM - HIV Infection, Ageing, Inflammation and Comorbidities. Prof. Brigitte Autran, December 2016.
(3) Marcus JL et al. Comparison of Overall and Comorbidity-Free Life Expectancy Between Insured Adults With and Without HIV Infection, 2000-2016. JAMA Network Open, 3: e207954, June 2020.